The term ‘obesity’ is used in this blog because it is the term commonly found in the research literature. However, we acknowledge that this term can be highly stigmatizing and may not fully capture the complexity of individual experiences with weight. We encourage a more nuanced understanding of health that goes beyond labels and recognizes the diverse factors that contribute to a person’s well-being.
What is leptin?
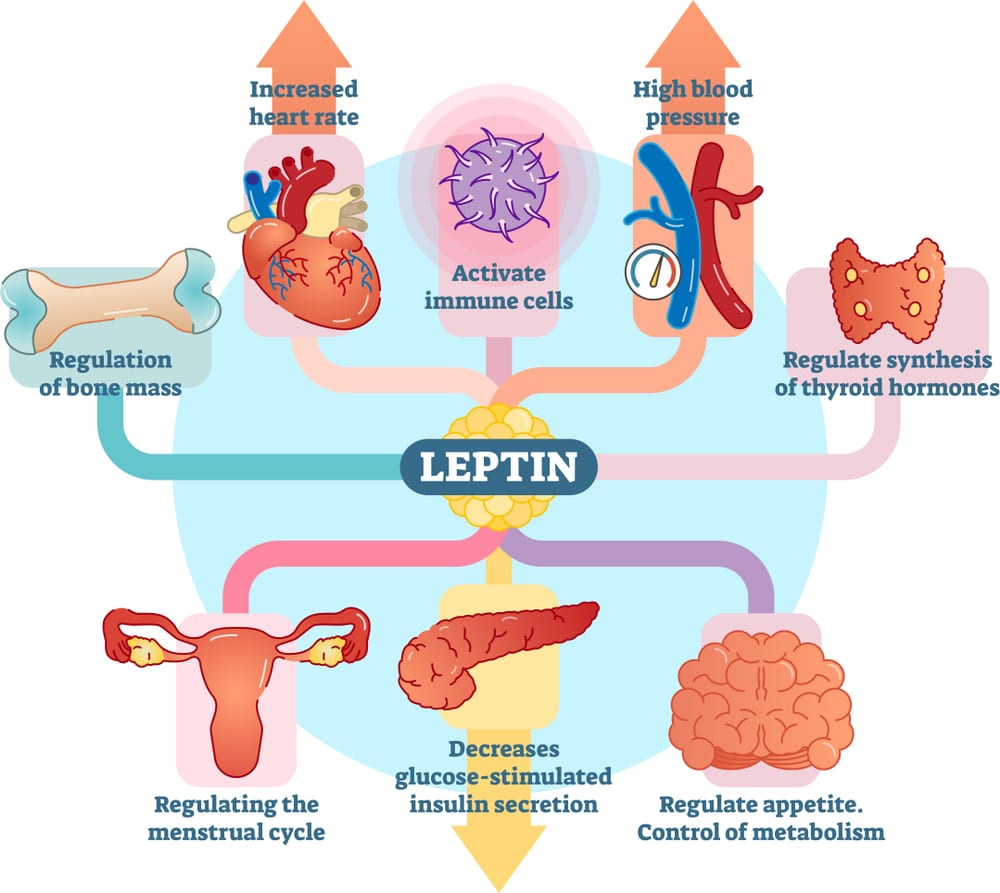
Leptin, often referred to as the “satiety” hormone, plays a critical role in regulating hunger, energy balance, and body weight.1 Leptin is a hormone produced by the adipose (fat) cells and signals to the brain when we have enough energy stored. This signaling helps to control our hunger and prevent overeating.
Though what happens when the body doesn’t produce enough leptin, or when the signals aren’t functioning properly? Leptin deficiency, as well as leptin resistance, can have significant impacts on our health.
What is leptin deficiency?
Leptin deficiency is a condition where the body doesn’t produce enough leptin. Genetic mutations that affect leptin production or its receptor are the most common cause of leptin deficiency. These genetic changes disrupt the body’s normal regulation of hunger and energy balance, and can lead to abnormal weight gain and other health issues. People with leptin deficiency may experience extreme hunger and a reduced ability to expend energy. Without enough leptin or a proper leptin response, the brain doesn’t get the message that the body has enough energy stores, which can result in a constant feeling of hunger. True leptin deficiency is rare, though leptin resistance, when the body doesn’t properly respond to the amount of leptin available, appears to be much more common.2
What is leptin resistance?
Leptin resistance occurs when the body produces enough leptin, but the brain doesn’t respond to it properly.2–4 In individuals where leptin is working properly, leptin signals the brain that the body has enough fat stored, which leads to a reduced appetite and increased energy expenditure. In leptin resistance, this signaling pathway is disrupted. The brain is “desensitized” to leptin, meaning leptin no longer effectively regulates hunger and energy balance. Individuals with leptin resistance may often experience chronic hunger, even though their body has plenty of energy reserves, leading to overeating and weight gain.
Leptin resistance is hypothesized to be one of the contributors to obesity. Individuals with higher levels of adiposity have been found to have high levels of leptin and are insensitive to the administration of leptin.2,4 Despite high levels of leptin, the brain is not effectively signaled to
stop eating, which can lead to a cycle of increased hunger and overeating. This phenomenon is outlined in Figure 1.

Figure 1. Relationship between obesity and leptin resistance. Adapted and modified from: Leptin, Obesity, and Leptin Resistance: Where Are We 25 years Later?5
Other ways leptin resistance can impact health
Leptin helps regulate immune function and is considered a proinflammatory cytokine.2,4 In its role as a proinflammatory cytokine,4 leptin may contribute to increased cardiovascular disease risk factors, including atherosclerosis, or the buildup of plaque in the arteries, and elevated lipid levels, or hyperlipidemia.2 Furthermore, leptin resistance may contribute to insulin resistance and diabetes.2 Leptin can inhibit the synthesis and secretion of insulin,6 a hormone needed for proper blood glucose management. Thus, leptin may have a role in the cardiovascular and diabetes related risks that are associated with higher levels of adiposity. This is depicted in Figure 2.
Leptin and eating disorders
The role of leptin and menstruation should also not be overlooked. Leptin, as a adipocytokine, plays a role in reproductive function, controlling the normal physiology of the female reproductive system. Rather than hyperleptinemia, which is seen in conditions associated with excess energy stores or metabolic disturbances, such as obesity,4,5 situations where nutritional status is suboptimal, such as disordered eating and eating disorders, are associated with low serum leptin levels.7 Leptin acts as a link between adipose tissue and the reproductive system, signaling whether adequate energy reserves are available for healthy reproductive function.7 Typically, leptin levels of 6-8 ng/mL are necessary to menstruate.

Figure 2. Relationship between leptin resistance and obesity-related cardiovascular disease. Adapted and modified from: Leptin Resistance2
What can be done about it?
While there is no one-size-fits-all solution for leptin resistance, several strategies have been shown to improve leptin sensitivity. High intensity exercise, in particular, has been shown to improve leptin sensitivity.8 In individuals with obesity, longer term (over 2 weeks) intakes of dietary fiber have been shown to lower serum leptin levels.9 Additionally, it is important to ensure adequate and sufficient sleep. Shorter sleep duration is associated with elevated leptin levels.10
Conclusions
Leptin deficiency and leptin resistance are two distinct but important conditions that affect hunger, metabolism, and overall health. Leptin deficiency is rare and caused by genetic mutations, while leptin resistance is more common and often associated with obesity, inflammation, and other lifestyle factors. Both conditions can lead to significant challenges in weight management and overall well-being.
By understanding how leptin works in the body and the factors that influence its function, individuals can take steps to manage leptin resistance and improve their health.
If you suspect you might be dealing with leptin resistance or deficiency, it’s important to consult with a healthcare provider for proper diagnosis and treatment options. The team at Laura Cipullo Whole Nutrition + Yoga is here to support.
References
- Tan HL, Yin L, Tan Y, et al. Leptin-activated hypothalamic BNC2 neurons acutely suppress food intake. Nature. 2024;636(8041):198-205. doi:10.1038/s41586-024-08108-2
- Martin SS, Qasim A, Reilly MP. Leptin Resistance. J Am Coll Cardiol. 2008;52(15):1201- 1210. doi:10.1016/j.jacc.2008.05.060
- Flier JS, Ahima RS. Leptin physiology and pathophysiology: knowns and unknowns 30 years after its discovery. J Clin Invest. 2024;134(1):e174595. doi:10.1172/JCI174595
- Gruzdeva O, Borodkina D, Uchasova E, Dyleva Y, Barbarash O. Leptin resistance: underlying mechanisms and diagnosis. Diabetes Metab Syndr Obes Targets Ther. 2019;Volume 12:191- 198. doi:10.2147/DMSO.S182406
- Izquierdo AG, Crujeiras AB, Casanueva FF, Carreira MC. Leptin, Obesity, and Leptin Resistance: Where Are We 25 Years Later? Nutrients. 2019;11(11):2704.
doi:10.3390/nu11112704
- Dagogo-Jack S. Leptin and Insulin Sensitivity: Endogenous Signals of Metabolic Homeostasis. J Clin Endocrinol Metab. 2024;109(5):e1402-e1403.
doi:10.1210/clinem/dgad653
- Moschos S, Chan JL, Mantzoros CS. Leptin and reproduction: a review. Fertil Steril. 2002;77(3):433-444. doi:10.1016/S0015-0282(01)03010-2
- De Assis GG, Murawska-Ciałowicz E. Exercise and Weight Management: The Role of Leptin—A Systematic Review and Update of Clinical Data from 2000–2022. J Clin Med. 2023;12(13):4490. doi:10.3390/jcm12134490
- Hassanzadeh-Rostami Z, Faghih S. Effect of Dietary Fiber on Serum Leptin Level: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Exp Clin Endocrinol Diabetes. 2021;129(04):322-333. doi:10.1055/a-0998-3883
10. Mosavat M, Mirsanjari M, Arabiat D, Smyth A, Whitehead L. The Role of Sleep Curtailment on Leptin Levels in Obesity and Diabetes Mellitus. Obes Facts. 2021;14(2):214- 221. doi:10.1159/000514095