Understanding Dysautonomia: What It Is, Causes, Symptoms, and Treatments
Have you ever wondered why your heart races when you’re scared or why your stomach churns during stressful moments? These reactions are all controlled by the autonomic nervous system (ANS), a critical part of our bodies that often goes unnoticed—until something goes wrong. In this blog, we will explore autonomic disorders, also known as autonomic neuropathy or dysautonomia, and how the way you eat can impact the condition.
What is the Autonomic Nervous System (ANS)?
The ANS regulates the things your body controls without conscious thought, like heart rate, blood pressure, digestion, and body temperature. The ANS consists of three components: the sympathetic nervous system (SNS), the parasympathetic nervous system (PNS), and the enteric nervous system (ENS). Most organs have nerves connected to these systems to control your body’s daily activities.
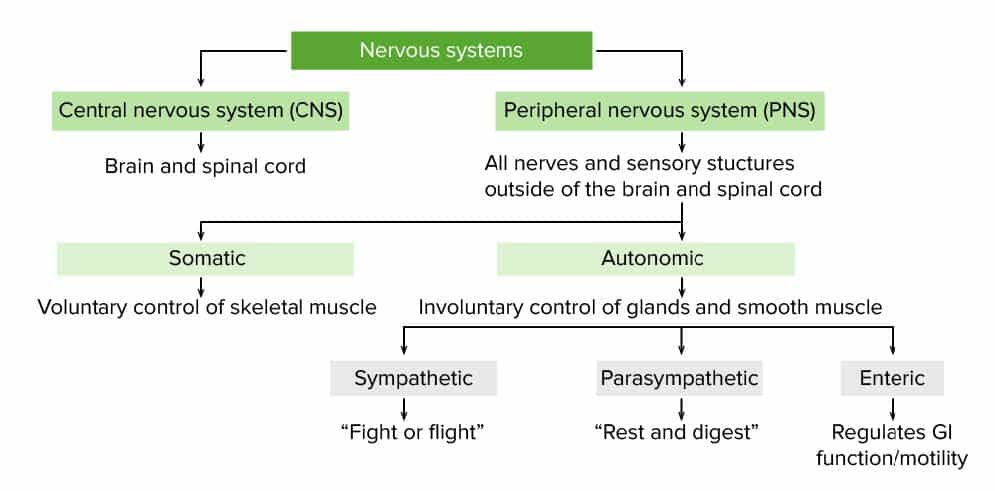
Figure 1: A diagram of the Nervous System. Photo cred: Lecturio
The Sympathetic Nervous System (SNS)
The SNS acts as the “fight or flight” response, preparing your body for stressful events, by raising your blood pressure and heart rate and slowing your digestive and urinary tract.
The Parasympathetic Nervous System (PNS)
The PNS has the opposite effect, helping your body relax after stress by lowering your blood pressure and heart rate and restarting digestion and urination.
The Enteric Nervous System (ENS)
The ENS oversees digestion, helping mix and move food through your intestines, support immune function, and remove toxic substances. It also increases blood flow to the intestines to improve the absorption and distribution of nutrients.
Understanding Autonomic Dysfunction
Autonomic dysfunction occurs when the nerves of the ANS are damaged, leading to a wide range of symptoms, from lightheadedness and fluctuating blood pressure to digestive issues and urinary problems. This damage can be caused by chronic conditions like Parkinson’s disease or diabetes, certain medications, injuries, and other factors such as:
- Autoimmune disorders
- Infections
- Long-term heavy drinking
- Physical Trauma
- Poisons and toxins
- Tumors
- Uncontrolled high blood pressure, and more
Common autonomic disorders include orthostatic hypotension, postprandial hypotension, multiple system atrophy, pure autonomic failure, afferent baroreflex failure, and familial dysautonomia.
How does the Autonomic Nervous System affect Digestion?
The ENS controls many of the necessary functions of the digestive system so we can absorb nutrients and expel harmful substances. When it does not work properly, your body cannot get the nutrients it needs to function, which can cause uncomfortable symptoms. Damage to the ENS can cause problems, such as:
- Loss of Appetite
- Bloating
- Diarrhea
- Constipation
- Difficulty Swallowing
Dysautonomia and Ehlers Danlos Syndrome (EDS)
Ehlers Danlos Syndrome (EDS) is a group of 13 heritable connective tissue disorders, each with its own unique diagnostic criteria. The main signs and symptoms seen across all types of EDS are fragile tissue, hyperelasticity of the skin, and joint hypermobility.
Many people with EDS also have some type of dysautonomia, experiencing some of the listed symptoms above. Often, those with EDS have orthostatic intolerance, which means they experience symptoms while standing up. The most common types of orthostatic intolerance are:
- Orthostatic hypotension (OH): low blood pressure when standing upright
- Postural orthostatic tachycardia syndrome (POTS): an abnormal increase in heart rate when standing without a drop in blood pressure
These conditions can be serious, as fainting can cause people to fall and break bones and joints, or hit their head.
Living With Dysautonomia: Diet and Lifestyle Recommendations
Most importantly, recommendations for autonomic dysfunction are individualized. They can vary depending on the type of autonomic disorder and by person. Some science-backed dietary recommendations include:
- Small, more frequent meals: After eating, blood is brought to the stomach to help absorb nutrients from digested food. Large meals can worsen symptoms like dizziness or lightheadedness.
- High (Soluable) Fiber Diet: Fiber can help reduce GI symptoms like constipation and bloating.
- Alcohol and Caffeine: Both of these substances can be dehydrating. It is recommended to limit and avoid alcohol. Caffeine, on the other hand, can help some individuals feel better, while it can make others feel jittery and raise their heart rate.
- Gluten-Free Diet: While not everyone needs to avoid it, some have reported that avoiding gluten improved their symptoms of autonomic dysfunction. However, there is no decisive conclusion on this recommendation.
- High-Salt, High-Fluid Diet: A high-salt diet might sound contradictory, but combining it with a high-fluid diet can help regulate heart rate and blood pressure symptoms.
Some lifestyle recommendations include:
- Elevated Head While Sleeping: Elevating your head four to six inches can reduce high blood pressure while lying down, which lessens the need to use the bathroom at night and maintain blood volume.
- Compression Garments: Compression stockings and abdominal compression garments can help prevent blood from pooling in the lower extremities and abdomen. However, research suggests that for these garments to be effective, they must extend to the top of the thighs and preferably to the abdomen.
- Physical Counter Maneuvers: Certain movements, like crossing your legs, muscle tensing, and squatting are effective ways to prevent fainting and dizziness.
- Drinking Water Before Getting Out Of Bed: Drinking water can help your body rehydrate and increase blood volume before getting up, so you are less likely to feel faint when standing.
More information on dietary and lifestyle recommendations can be found here.
Resources and Conclusions
Autonomic dysfunction encompasses a range of conditions with diverse symptoms and treatments. These symptoms can be mild or life-threatening, making it imperative to have a strong medical team and support group behind you. Consider joining support groups, either locally or online. Resources like the Dysautonomia International and The Ehlers Danlos Society websites can provide additional information and research updates.
Are you struggling with digestive symptoms or other autonomic disorder issues? You can schedule an appointment with one of our expert dietitians and start your journey to better health with personalized care.
References
Autonomic Nervous System: What it is, Function & Disorders. Cleveland Clinic. (n.d.). https://my.clevelandclinic.org/health/body/23273-autonomic-nervous-system
Bryarly, M., Phillips, L. T., Fu, Q., Vernino, S., & Levine, B. D. (2019). Postural orthostatic tachycardia syndrome. Journal of the American College of Cardiology, 73(10), 1207–1228. https://doi.org/10.1016/j.jacc.2018.11.059
Case-Lo, C. (2019, March 8). Autonomic dysfunction: Symptoms, types, and treatments. Healthline. https://www.healthline.com/health/autonomic-dysfunction#TOC_TITLE_HDR_1
Diet & Nutrition. (2021). Dysautonomia Support Network. https://www.dysautonomiasupport.org/diet-nutrition/
Dysautonomia. The Ehlers Danlos Society. (2024, May 7). https://www.ehlers-danlos.com/dysautonomia/
Fleming, M. A., Ehsan, L., Moore, S. R., & Levin, D. E. (2020). The Enteric Nervous System and its Emerging Role as a Therapeutic Target. Gastroenterology Research and Practice, 2020, 1–13. https://doi.org/10.1155/2020/8024171
Mayo Clinic Staff. (2022, July 7). Autonomic neuropathy. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/autonomic-neuropathy/diagnosis-treatment/drc-20369836
Types of Autonomic Disorders. NYU Langone Health. (n.d.). https://nyulangone.org/conditions/autonomic-disorders/types