Most often in our practice, we treat our clients who present with an ARFID diagnosis with Cognitive-Behavioral Therapy for ARFID, also known as CBT-AR1 (as well as Laura and Paige’s sprinkle of knowledge and training from the SOS Approach to Feeding).
ARFID is defined by the DSM-5 Criteria2 as:
- An eating or feeding disturbance (e.g., apparent lack of interest in eating or food; avoidance based on the sensory characteristics of food; concern about aversive consequences of eating) as manifested by persistent failure to meet appropriate nutritional and/or energy needs associated with one (or more) of the following:
- Significant weight loss (or failure to achieve expected weight gain or faltering growth in children)
- Significant nutritional deficiency.
- Dependence on enteral feeding or oral nutritional supplements.
- Marked interference with psychosocial functioning.
- The eating disturbance is not attributable to a concurrent medical condition or not better explained by another mental disorder. When the eating disturbance occurs in the context of another mental disorder, the severity of the eating disturbance exceeds that routinely associated with the condition or disorder and warrants additional clinical attention.
- The disturbance is not better explained by lack of available food or by an associated culturally sanctioned practice.
- The eating disturbance does not occur exclusively during the course of anorexia nervosa or bulimia nervosa, and there is no evidence of a disturbance in the way in which one’s body weight or shape is experienced.
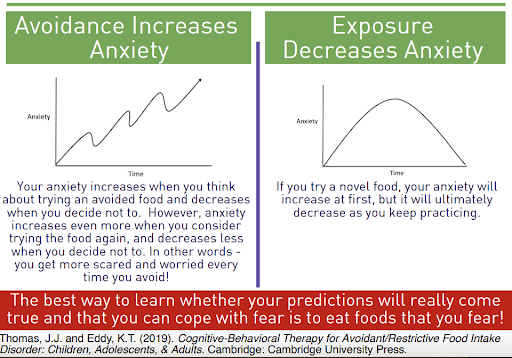
Avoidance is Only a Temporary Solution
Avoidance of certain food groups, textures, flavors, smells, etc. in an individual with ARFID only is a temporary solution to their anxiety. The longer one avoids the heightened the anxiety, the more coping strategies needed to regulate. It is important to understand that an individual with ARFID is not just being difficult, picky or stubborn. This is a true biological wiring in which requires unlearning their learned adaptive behaviors. This individual may be using adaptive behaviors such as small bites, chewing for much longer than necessary, only eating “safe” foods in an exactly specific way, or even not eating at all as a way to cope with their discomfort or lack of sensory regulation. In order to interrupt such avoidant behaviors, we must “test the hypothesis”, in other words, do the scary thing to see that the negative prediction is not always the factual outcome. The most tried and true way to tackle this in treatment is exposure therapy. The best way to overcome the fear is to work on exposures to such fears in a planned and systematic way. We do this is by creating a food exposure hierarchy. Within the first few sessions with our clients, we will assist them and their families in creating an exposure hierarchy, an plan out one at a time, facing these fears and aversions.
Creating an Exposure Hierarchy
To create your own exposure hierarchy, you will rank you food fears from least anxiety provoking to most anxiety provoking using a scale from 1-100, called subject units of distress. Pending the age of the client we may narrow this range such as 1-10, or using colors. It is most important for the individual to create a ranking system that resonates with them and they can understand. We recommend moving at the pace the individual is ready for, starting with lower ranked, easier, foods and progressing to more challenging ones with increasing trust and comfortability.
Download our template and give it a try. Working with a registered dietitian and multidisciplinary team to work through the thoughts, feelings and behaviors that come up around these food fears as you try moving up this ladder is the best way to make sustainable and meaningful progress.
References
- Kambanis PE, Breithaupt L, Zayas L, Eddy KT, Thomas JJ. Cognitive-Behavioral Therapy for Avoidant/Restrictive Food Intake Disorder (CBT-AR). In: Sprich SE, Petersen T, Wilhelm S, eds. The Massachusetts General Hospital Handbook of Cognitive Behavioral Therapy. Current Clinical Psychiatry. Springer International Publishing; 2023:247-258. doi:10.1007/978-3-031-29368-9_17
- Administration SA and MHS. Table 22, DSM-IV to DSM-5 Avoidant/Restrictive Food Intake Disorder Comparison. June 2016. Accessed August 8, 2024. https://www.ncbi.nlm.nih.gov/books/NBK519712/table/ch3.t18/









